Prior Authorization Certification
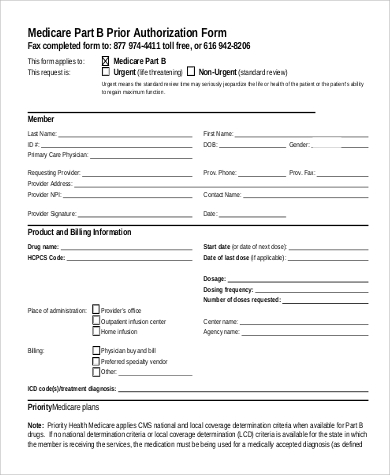
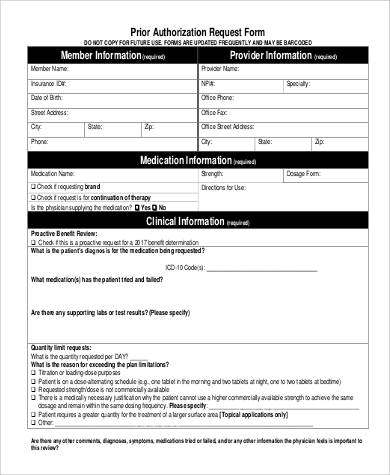
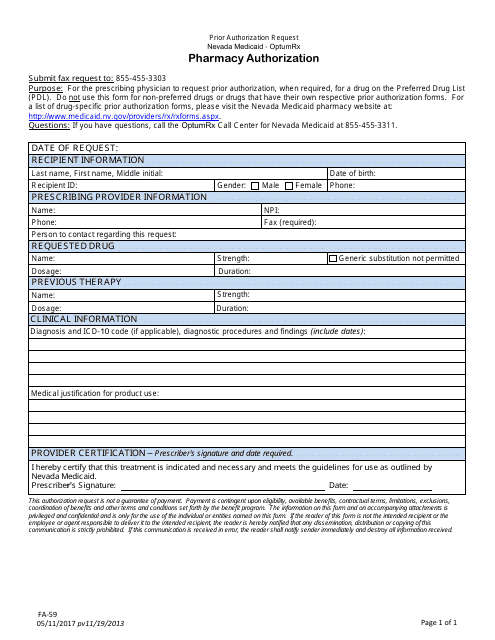
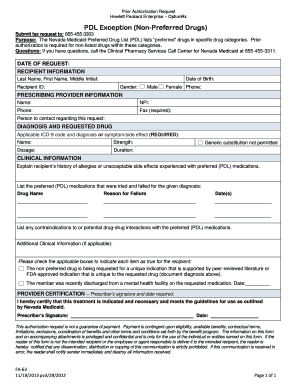
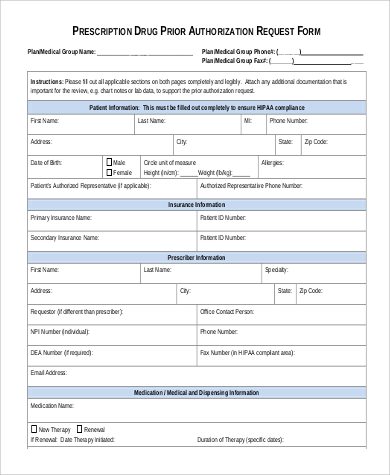
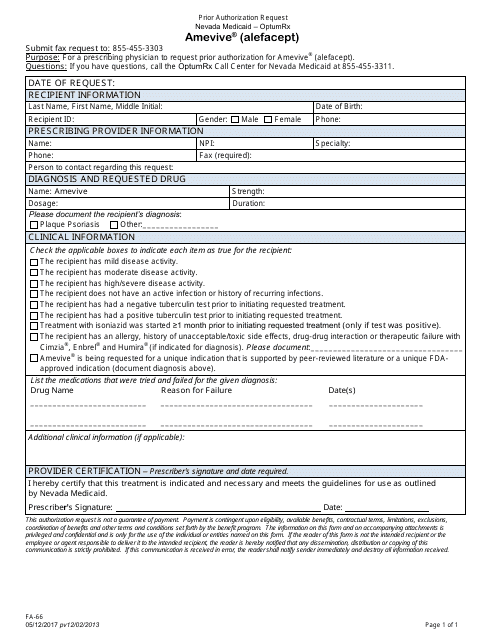
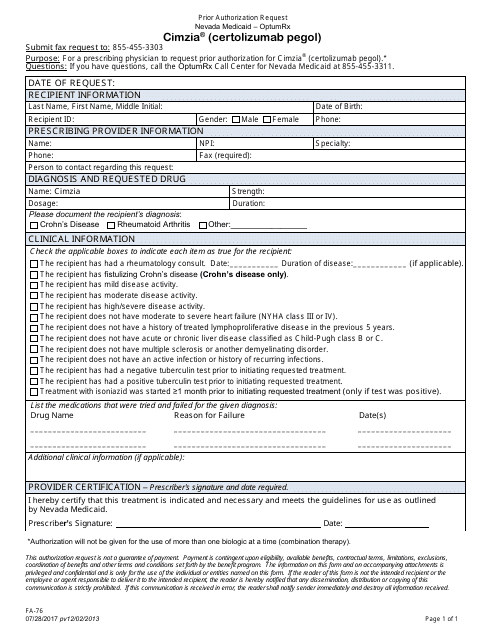
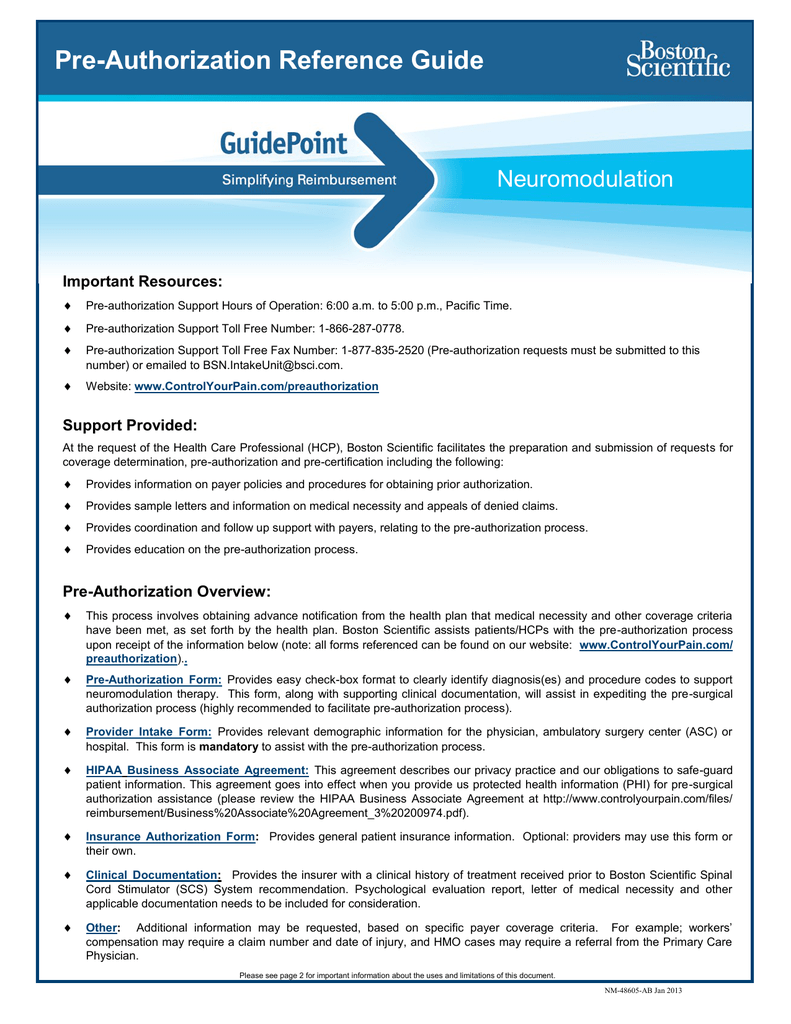
Pre certification a pre certification requirement means that a payer must review the medical necessity of a proposed service and provide a certification number before a claim will be paid.
Prior authorization certification. Pre certification prior authorization pre determination these processes are a cost containment feature of many group medical policies whereby the insured must contact the insurer prior to a hospitalization or surgery and receive authorization for the service. Prior authorization is a requirement that your physician obtain approval from your health plan to prescribe a specific medication for you. Failure to receive preadmission certification usually involves a penalty payment by the member of a specified dollar amount varies by plan design. Prior authorization health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre approval pre authorization and pre certification.
For pharmacists medical insurance medical billing medical coding and healthcare administrators. Without this prior approval your health plan may not provide coverage or pay for your medication. Weve provided the following resources to help you understand anthems prior authorization process and obtain authorization for your patients when its required. Authorization can be granted retroactively for example a patient or hospital may have a 24 hour window to notify a payer after receiving emergency care.